 62.86% Blame the U.K. Government for the Rising Suicide Rates Among Doctors
62.86% Blame the U.K. Government for the Rising Suicide Rates Among DoctorsIn a distressing development, suicide among doctors in the U.K. has seen a significant rise, shedding light on the dire challenges faced by medical professionals. The story of Jagdip Sidhu, an accomplished doctor who tragically took his own life, highlights the immense pressures doctors contend with. Factors such as high workloads and inadequate support structures have come to the forefront as contributors to this concerning trend.
Efforts to address the high suicide rate among doctors have been initiated, with organizations and individuals working to provide crucial mental health support for healthcare professionals.
It’s becoming increasingly evident that a systemic shift within the medical community is essential to avert further tragedies. The impact of funding cuts, exacerbated by the COVID-19 pandemic, and the pervasive culture within the medical field are also being scrutinized as factors that exacerbate this grave societal issue.
Real Research, an online survey app, launched a survey on suicide rate among doctors rising alarmingly to gauge public perceptions of the rise in suicides among U.K. doctors.
Highlights:
- 62.86% said it was the U.K. government’s responsibility for suicide among doctors.
- 44.09% feel the public’s perspective of healthcare workers is somewhat ethical.
- Work standards for healthcare workers are somewhat justified, reported 45.93%.
In the United Kingdom, a stark and disconcerting picture has emerged, shedding light on the distressing plight that doctors find themselves grappling with. Recent studies have uncovered an alarming trend: an increasing number of doctors are tragically succumbing to suicide.
Awareness and Factors Revealed
According to the survey on suicide among doctors, most respondents (42%) were well aware of the suicide rate among doctors in the U.K., while 35.36% had a vague awareness, and 22.64% were completely unaware.
Amid the labyrinth of contributing factors, the burden of overwhelming workloads, instances of workplace harassment, and the absence of robust support systems stand out prominently. 57.98% of respondents were aware that doctors in the U.K. face high-pressure workloads, bullying, and poor support structures, while 42.02% were not.
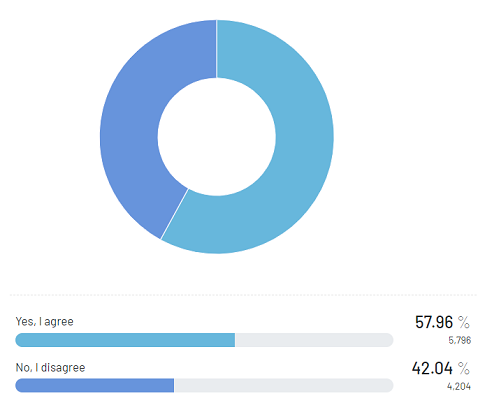
Furthermore, at the heart of this discussion lies the palpable pressure experienced by doctors in their professional capacities. The expectations placed upon them are nothing short of extraordinary, sparking a contentious debate about the reasonableness of these demands. When asked about the “golden dream” of a secure future at the cost of one’s mental and physical health, 57.96% agreed, compared to 42.02% who disagreed.
Examining Public Expectations of Medical Practitioners
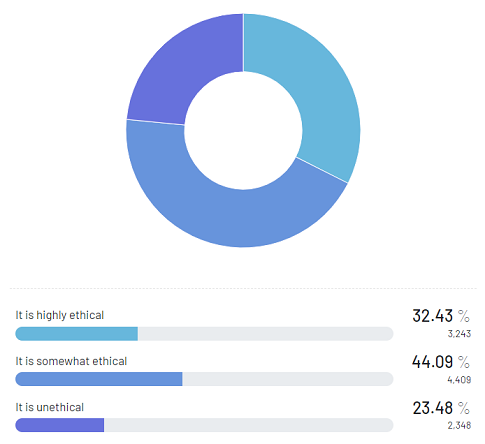
Parallel to these challenges is the societal perception of doctors, often held on a pedestal as unyielding pillars of strength. This perspective prompts a crucial ethical inquiry: Is it equitable to maintain such lofty expectations and heap relentless pressure on medical practitioners?
The survey reveals a divided stance. About 32.43% of respondents said the general public’s perspective on health professionals expecting superhuman levels of work and resilience is highly ethical, while 44.09% considered it somewhat ethical, and 23.48% deemed it unethical.
The government’s role in exacerbating or alleviating this crisis is a critical piece of the puzzle. Budgetary constraints have led to an insufficient workforce, intensifying the burden on doctors and, tragically, contributing to the rising suicide among doctors.
The public sentiment is unmistakable; a substantial majority (62.86%) believes in the government’s responsibility to prioritize the mental and physical well-being of medical professionals, while 37.14% think otherwise.
Experiences of Expat Doctors in the UK Amidst Mental Strain
Amidst the disquieting surge in the suicide among doctors in the U.K., a concerning gender disparity comes to light. Expat female doctors in the country, grappling with mental breakdowns and burnout, emerge as the vulnerable cohort.
Based on the poll results, 54.29% of the respondents agreed that expat female doctors endure a harsher reality compared to their male counterparts. This sentiment gains further traction with 22.67% strongly agreeing, while 20.69% and 2.35% disagreed and strongly disagreed, respectively.
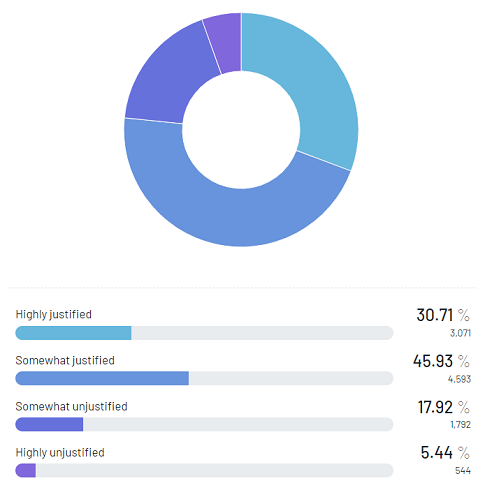
As the medical realm’s demanding nature persists, a disconcerting inquiry surfaces regarding the standards to which healthcare practitioners are held. 30.71% of respondents assert that the high standards and inhumane levels of proficiency expected from medics are highly justified.
Furthermore, 45.93% opined that these standards hold some degree of justification, underscoring the complexity of the issue. However, a notable segment, comprising 17.92%, regarded them as somewhat unjustified, shedding light on the prevalent reservations. The remaining 5.44% found these standards to be highly unjustified.
Methodology | |
| Survey Title | Survey on Suicide Rate Among Doctors Rising Alarmingly |
| Duration | August 3, 2023 – August 10, 2023 |
| Number of Participants | 10,000 |
| Demographics | Males and females, aged 21 to 99 |
| Participating Countries | Afghanistan, Algeria, Angola, Argentina, Armenia, Australia, Azerbaijan, Bahrain, Bangladesh, Belarus, Benin, Bolivia,… Brazil, Brunei, Bulgaria, Burkina Faso, Cambodia, Cameroon, Canada, Chile, China, China (Hong Kong) China (Macao), China (Taiwan), Colombia, Costa Rica, Croatia, Czech Republic, Ecuador, Egypt, El Salvador, Ethiopia, Finland, France, Gambia, Georgia, Germany, Ghana, Greece, Greanada, Guatemala, Honduras, Hungary, India, Indonesia, Iraq, Ireland, Israel, Italy, Ivory Coast, Japan, Jordan, Kenya, Kuwait, Kyrgyzstan, Latvia, Lebanon, Libya, Lithuania, Malaysia, Maldives, Maluritania, Mexico, Moldova, Mongolia, Morocco, Mozambique, Myanmar [Burma], Namibia, Nepal, Nicaragua, Nigeria, Oman, Pakistan, Palestine, Panama, Peru, Philippines, Poland, Portugal, Qatar, Romania, Russia, Saudi Arabia, Serbia, Sierra Leone, Singapore, Slovakia, South Africa, South Korea, Spain, Sri Lanka, Tanzania, Thailand, Togo, Tunisia, Turkey, Turkmenistan, Uganda, Ukraine, United Arab Emirates, United Kingdom, United States, Uruguay, Uzbekistan, Venezuela, Vietnam, Yemen, Zimbabwe. |
RR Author
Real Research News is the media platform that presents insights and studies of wide-range of topics. It focuses on insights gathered from its survey app.







